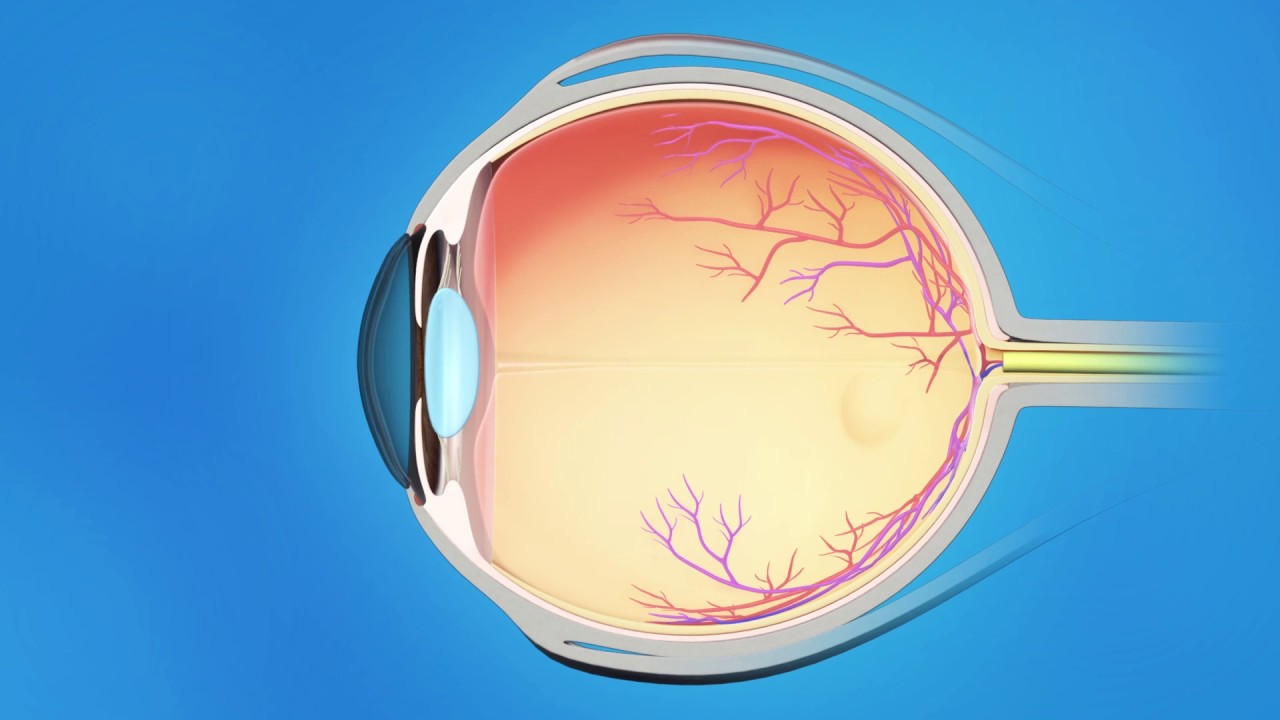
Glaucoma is a term that is used to describe a broad range of eye problems that can damage the optic nerve and cause loss of vision. The pressure inside the eye, called Intraocular Pressure (IOP), generally falls within a range that is considered “normal.” When IOP is not in the normal range, it may be due to one of the types of Glaucoma.

Regardless of type, if not diagnosed early, treated properly, and controlled, Glaucoma will result in permanent vision loss and potentially blindness. Dr. Spector is a Fellowship trained Glaucoma specialist and provides comprehensive diagnostic testing and treatment for Glaucoma.
Diagnosis
The best way to maintain eye health and preserve your vision is to have regular and complete eye examinations with the appropriate level of diagnostic testing for Glaucoma. During your examination, Dr. Spector and the staff may perform a number of tests in order to make the most accurate diagnosis of Glaucoma. These include the following testing procedures:
Tonometry
The Tonometry Test is a method of measuring your Intraocular Pressure (IOP). This test involves first placing some eye drops into your eyes to numb them, then lightly touching the surface of the Cornea with a specialized measuring instrument. There is no discomfort involved. The test is quick and gives Dr. Spector the first piece of important information in determining whether you have Glaucoma.
Ophthalmoscopy
Ophthalmoscopy is a method of carefully examining the inside of the eye, especially the optic nerve, in order to detect Glaucoma. Some eye drops will be placed in your eyes in order to dilate your pupils so that Dr. Spector can make a clear and direct observation of the optic nerve. The examination will take place in a darkened room using different types of Ophthalmoscopes in order to examine the shape and color of your optic nerve. If either the Intraocular Pressure (IOP) is elevated or the optic nerve appears unusual, additional tests will be necessary in order to complete the Glaucoma examination.
Visual Field Perimetry
Perimetry or Visual Field testing is an important part of the Glaucoma examination. During this test you will be asked to sit in front of a large “bowl like” instrument and look straight ahead. A computer program will present a number of lights in different positions of their “side” or peripheral vision to see how sensitive your side vision is in various directions. The computer will then plot an actual map of the field of vision so that Dr. Spector can interpret this map in conjunction with other examination tests in order to understand how well the optic nerve is functioning. Glaucoma usually affects your side vision before your central vision, so visual field testing can often show any problems from glaucoma before you can notice them.
Gonioscopy
The Optic Nerve Computer Imaging System at Spector Eye Care is called OCT. The OCT uses a method called “optical coherence tomography” that is capable of creating digital images through the use of special beams of light to create a contour map of the optic nerve and measure the retinal nerve fiber thickness. In many regards, this is similar to the CT Scans used to study organ systems and tissues throughout your body.
The goal of OCT Optic Nerve Computer Imaging is to give Dr. Spector the ability to detect the slightest loss of optic nerve fibers in order to diagnose Glaucoma at the earliest possible stage and stop the progression of the disease.
What People Say About Us!
Dr. Spector was wonderful. He saw our daughter as an emergency over a holiday weekend even though we aren’t current patients of his practice (we absolutely will be after this!). He was super responsive and called periodically to check up on her. He was caring and took the time to answer all our questions and concerns. True professional
Pachymetry Measurement of Corneal Thickness
The Pachymetry Test is a simple, quick and painless way of accurately measuring your coneal thickness. Corneal thickness is important because it can alter the accuracy of the measurement of Intraocular Pressure, potentially causing doctors to treat you for a condition that may not exist. Your actual Intraocular Pressure may be UNDERESTIMATED if you have thin corneas and it may be OVERESTIMATED if you have thicker corneas. During a Glaucoma examination, Dr. Spector or a staff member may perform a Pachymetry Test to measure your corneal thickness and consider this finding to make the most accurate diagnosis. The test is performed by first placing some drops in your eyes to make them numb and then lighty touching the cornea with a “pencil like” probe that uses sound waves to precisely measure your corneal thickness.
Treatment
Glaucoma has no cure, but in almost all cases, it is treatable if caught early. As a Glaucoma Specialist, there are three main methods that Dr. Spector can use to treat Glaucoma: Medical, Laser and Surgical.
Medical Treatment of Glaucoma
Primary Open Angle Glaucoma is most often treated with eye drops. There are many types of eye drops that can be prescribed to lower Intraocular Pressure (IOP). By using a single type of medication or sometimes 2 eye drops in combination, more than 80% of the patients with Open Angle Glaucoma can be successfully treated. These eye drops work by either decreasing the amount of fluid being produced inside your eye or by increasing the rate of drainage of fluid from your eye. For most patients, by using the eye drops as prescribed it is possible to control the Intraocular Pressure (IOP) and slow or even halt the loss of vision.
Unfortunately, some patients may experience side effects from these eye drops making the use of eye drops a poor treatment option. Also, some patients are unable to achieve adequate control with eye drops alone and require Laser Treatment for Glaucoma in addition to the eye drops in order to maintain control.
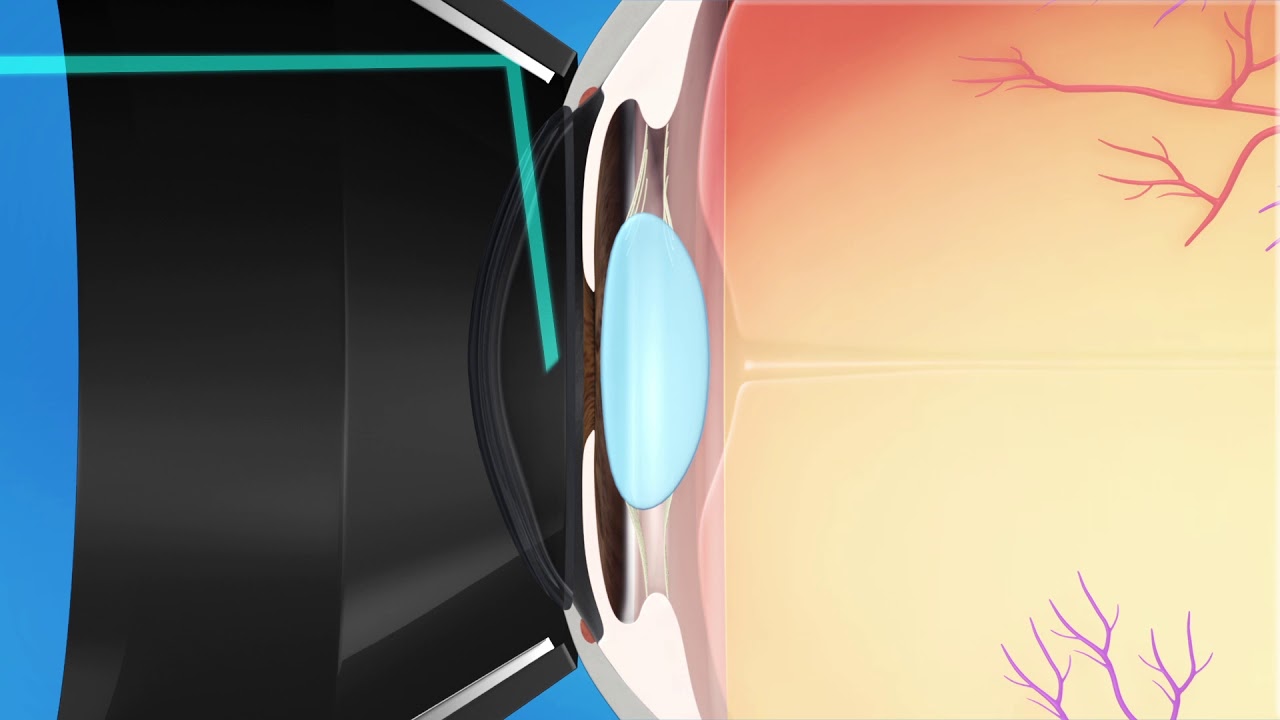
Laser Treatment of Glaucoma

Dr. Spector has found that the use of Laser Treatment for Glaucoma has become an important option for many patients. In the past, Laser Eye Surgery for Glaucoma was considered a “last resort” before Glaucoma Surgery. Today, thanks to advances in lasers, using a laser treatment for Glaucoma in conjunction with the eye drop treatment or sometimes even using the Laser Treatment as the primary treatment are excellent options to help maintain control and slow or stop the progression of the disease. Laser Treatment for Glaucoma is regularly used to help prevent vision loss and is becoming a Glaucoma treatment of choice for many patients who have problems with eye drops or are unable to use eye drops properly.
Argon Laser Trabeculoplasty (ALT) is a type of glaucoma laser treatment that helps to reduce the Intraocular Pressure (IOP) by creating more effective drainage of fluid through the Trabecular Meshwork. Unfortunately, for some patients, the effect of ALT decreases over time, rendering it ineffective. This is limiting, as ALT cannot usually be repeated.
Another type of Laser Treatment for Glaucoma is Selective Laser Trabeculoplasty (SLT). SLT may offer advantages over ALT for some patients because SLT can be repeated several times if needed to control the pressure and slow or halt the progression of the disease. SLT has promise in becoming an important treatment option not only for Glaucoma patients who are unable to use eye drops to obtain control, but as a primary treatment to help Glaucoma patients avoid needing to use eye drops altogether.
Surgical Treatment of Glaucoma
For a small number of patients, it is still not possible to achieve control of their disease and stop the progression of vision loss, even with the maximum medical therapy they can achieve with Glaucoma eye drops and Laser Eye Surgery.
For these patients Dr. Spector can perform a number of surgical procedures, including: Trabeculectomy, wherein a tiny piece of the Trabecular Meshwork is removed, Sclerostomy or “Filtering Procedure”, which removes a small piece of the sclera for drainage, or even implanting a microscopic Glaucoma Valve to help reduce and stabilize the Intraocular Pressure (IOP).